Americans have long understood the value of competition in improving the quality and value of the products we buy. Unfortunately, in health care, competition is not always present. And the lack of competition in the hospital industry is a big part of why American hospitals are the costliest in the world.
Bipartisan consensus
On Wednesday, November 20th, FREOPP and the Progressive Policy Institute (PPI) co-hosted a symposium on Capitol Hill on restoring competitive hospital markets, entitled Affordable Health Care Through Competition: Solutions from the Left and Right. FREOPP President
shared the stage with PPI’s Ben Ritz to discuss ideas bipartisan paths forward on restoring competition for hospital markets, with insightful commentary from Shawn Bishop, formerly of the Commonwealth Fund and the Senate Finance Committee. Fittingly, Marilyn Werber Serafini of the Bipartisan Policy Center moderated the discussion.
Amongst this consortium of political ideologies, uniform consensus emerged around the need for local hospital markets to remain competitive for patients to have access to more affordable care. As put forth in Roy’s white paper Improving Hospital Competition: A Key to Affordable Health Care, one of the key drivers of higher prices for hospital care is the rise of regional hospital monopolies. As small and medium sized hospitals merge into larger hospital systems, these new entities can use their increased market power to demand higher prices from the uninsured and privately insured alike.
More size means more power
As hospital systems have grown larger over time, so too has their bargaining power to charge higher prices to private insurers. While hospitals and private insurers have remained locked in an ongoing tug-of-war when negotiating prices, more often than not, the results of these efforts leads to increased prices relative to what the federal government pays for Medicare and Medicaid. Hospitals claim that this practice, known as “cost shifting,” is needed to help offset the losses incurred by accepting Medicare and Medicaid rates lower than the rates of private insurance. While this may have been true at one time, evidence shows that hospitals are today making money on all insured populations, and charging more to privately insured patients simply because they can. This trend been seen nationwide.
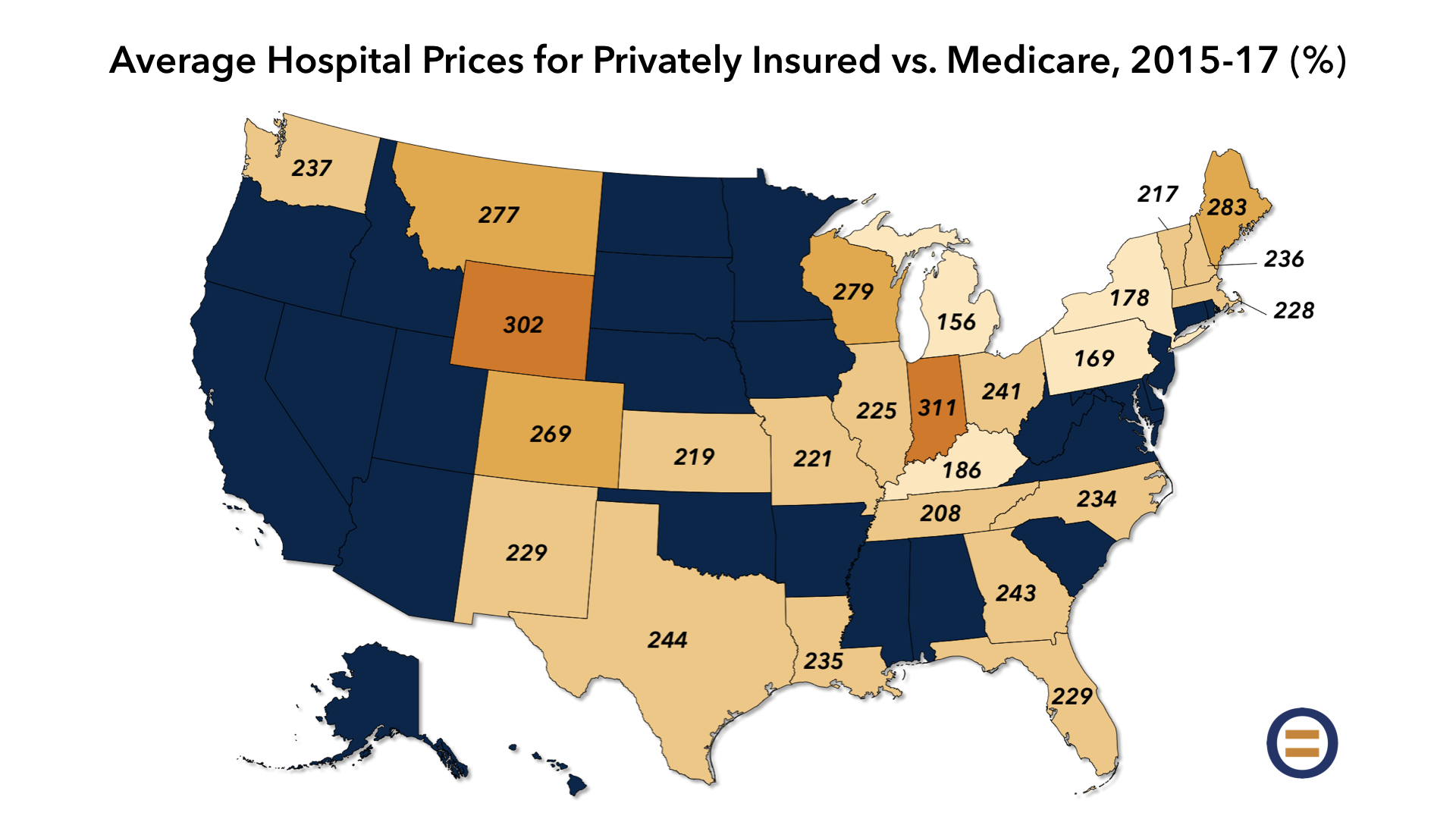
In a 2015 study by the U.S. Agency for Healthcare Research and Quality, researchers found that hospitals were charging private insurers 106.1 percent of Medicare rates in 1996, and 175.3 percent of Medicare rates in 2012. A similar 2019 study by the RAND Corporation found that, on average, hospitals in 25 states were charging private insurance 241 percent of Medicare rates in 2017. With no regulatory or market-based restraints in sight, it is likely that these trends will continue.
Admittedly, while percentage costs of Medicare can be hard to envision for the average patient, looking at specific medical procedures can help shed light on how this increased pricing power affects individuals. In 2011, Professor James Robinson of the University of California examined the hospital prices charged to private insurers for six common procedures: angioplasties, pacemaker insertions, knee replacements, hip replacements, lumbar fusions and cervical fusions. For hospital markets with above-average market consolidation, these procedures cost up to 44 percent more.
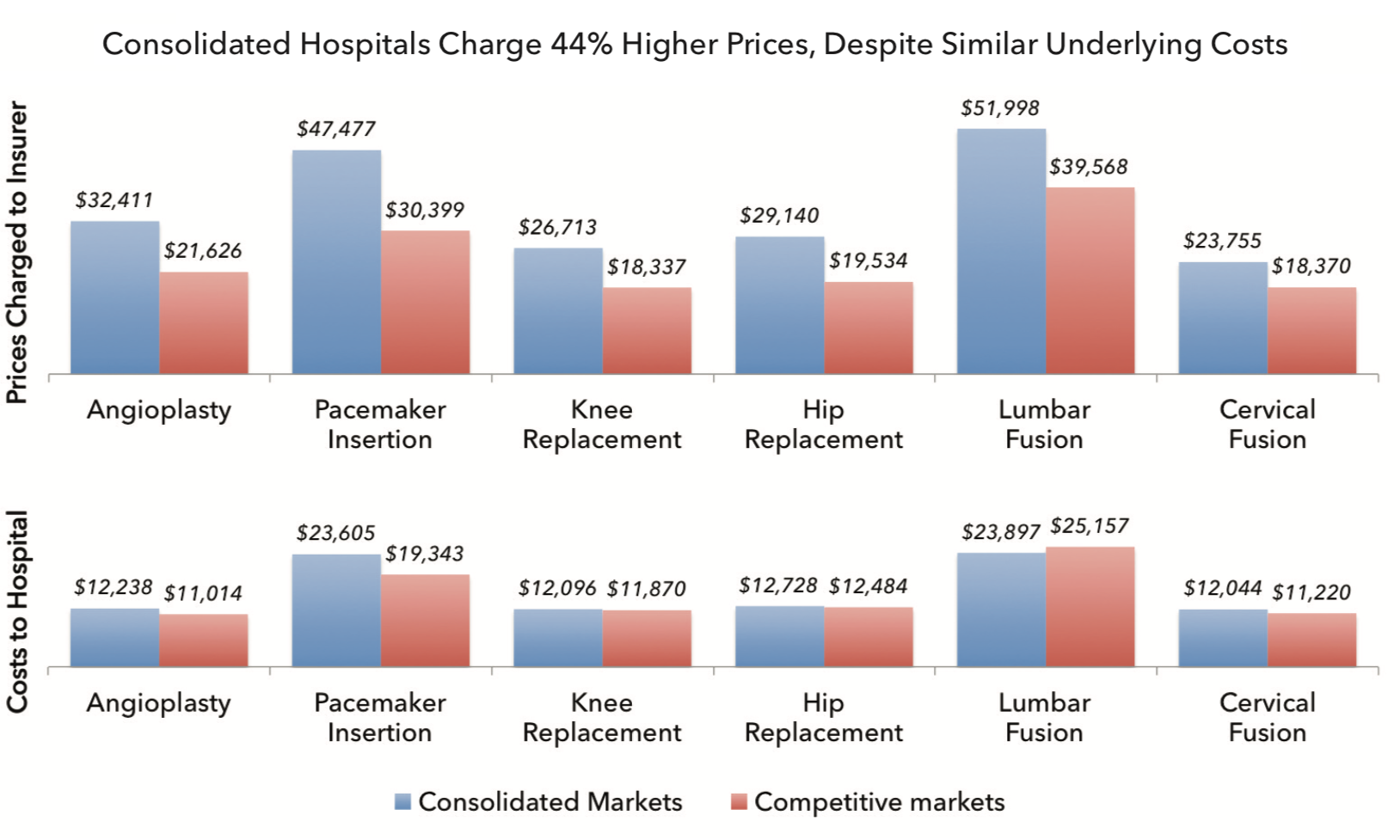
Using an angioplasty as an example, in competitive markets (the red bar), the average hospital charged $21,626; and in consolidated markets (the blue bar), the average hospital charged $32,411: a premium of 49.9 percent.
However, the average cost to both the hospital for performing the angioplasty was almost identical: $11,014 in competitive markets and $12,238 in consolidated markets.
The reason for this discrepancy stems from what is referred to as a “contribution margin.” From an economic standpoint, a contribution margin is a product’s price subtracted from its associated costs, resulting in a profit earned for each unit sold. In a medical context, this would be represented by each procedure performed with its billed charges to the insurer subtracted from the costs of performing the procedure incurred by the hospital. Thus, the higher the contribution margin, the larger the hospital’s profit. In the Robinson study, consolidated hospitals generated over two times the contribution margin as hospitals in competitive markets did. Clearly, from a contribution margin standpoint, as a hospital, bigger truly is better.
A more competitive future
As outlined in Improving Hospital Competition, there are various ways to encourage more competition within regional hospital markets, and in turn, help lower prices for patients. To do so, Roy proposes:
- Discouraging future hospital mergers by significantly expanding the Federal Trade Commission’s hospital antitrust staff, allowing the FTC to regulate anticompetitive practices by nonprofit hospitals, and publishing — on a quarterly basis — data for every ZIP code or region regarding hospital market concentration.
- Encouraging new hospital competition by encouraging states through federal grants to eliminate certificate of need laws, any willing provider laws, network adequacy requirements, certificate of public advantage laws, and similar provisions; removing the Affordable Care Act’s ban on new physician-owned hospital construction; and barring the deployment of hospital-led accountable care organizations in concentrated markets;
- Transforming price and contractual transparency through an all-payer claims database, and through a requirement for public disclosure of payer-provider contracts, so as to flush out anticompetitive practices;
- Facilitating medical tourism and telemedicine through harmonization of state medical licensing, reference pricing, and scope of practice laws; and
- Integrating Veterans Health Administration hospitals into the broader health care system by allowing private patients to use VA hospitals, and by allowing VA hospitals to compete on price with non-VA hospitals.
Moreover, unlike antitrust enforcement from the federal and state levels that would be punitive, perhaps extending the notion of choice to regional hospital monopolies could offer the best path forward. Regional monopolies could choose: (1) to remain consolidated but without practicing exploitative pricing power, or (2) voluntarily divest and restore a more competitive provider market in the region. In sum, the issue is not so much that hospitals are large, it is that they often become large for the sole purpose of increasing pricing power.
The benefits of improving hospital competition are manifold. Breaking up hospital monopolies will allow for more competitive pricing, which in turn, will help reduce the cost of U.S. healthcare nationally. As a result, hospitals will seek to innovate their infrastructure, patient services and medical technologies. Most importantly, improving hospital competition builds a more affordable health system for all Americans, and sets forth a more fiscally sustainable model for future generations.
